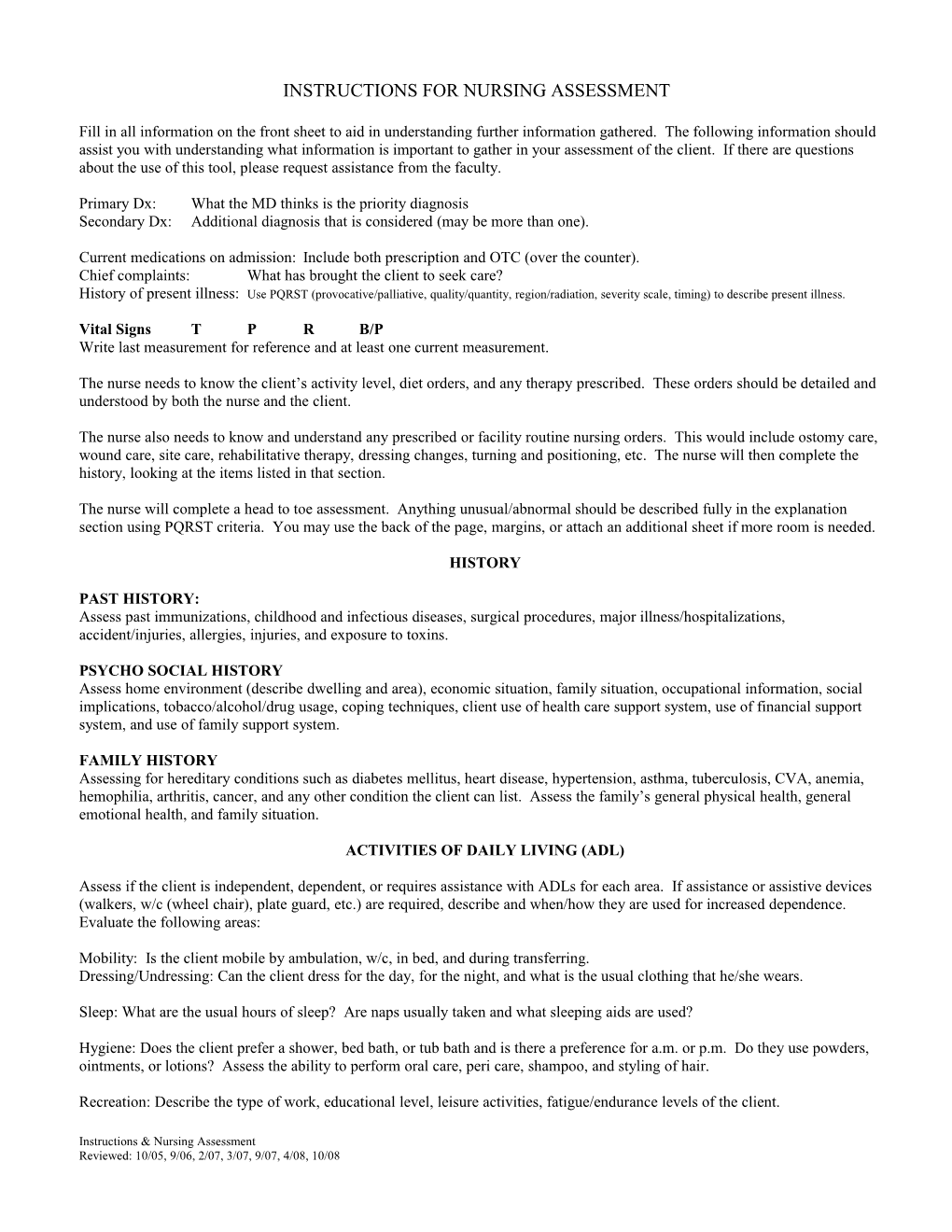
INSTRUCTIONS FOR NURSING ASSESSMENT
Fill in all information on the front sheet to aid in understanding further information gathered. The following information should assist you with understanding what information is important to gather in your assessment of the client. If there are questions about the use of this tool, please request assistance from the faculty.
Primary Dx: What the MD thinks is the priority diagnosis
Secondary Dx: Additional diagnosis that is considered (may be more than one).
Current medications on admission: Include both prescription and OTC (over the counter).
Chief complaints: What has brought the client to seek care?
History of present illness: Use PQRST (provocative/palliative, quality/quantity, region/radiation, severity scale, timing) to describe present illness.
Vital Signs T P R B/P
Write last measurement for reference and at least one current measurement.
The nurse needs to know the client’s activity level, diet orders, and any therapy prescribed. These orders should be detailed and understood by both the nurse and the client.
The nurse also needs to know and understand any prescribed or facility routine nursing orders. This would include ostomy care, wound care, site care, rehabilitative therapy, dressing changes, turning and positioning, etc. The nurse will then complete the history, looking at the items listed in that section.
The nurse will complete a head to toe assessment. Anything unusual/abnormal should be described fully in the explanation section using PQRST criteria. You may use the back of the page, margins, or attach an additional sheet if more room is needed.
HISTORY
PAST HISTORY:
Assess past immunizations, childhood and infectious diseases, surgical procedures, major illness/hospitalizations, accident/injuries, allergies, injuries, and exposure to toxins.
PSYCHO SOCIAL HISTORY
Assess home environment (describe dwelling and area), economic situation, family situation, occupational information, social implications, tobacco/alcohol/drug usage, coping techniques, client use of health care support system, use of financial support system, and use of family support system.
FAMILY HISTORY
Assessing for hereditary conditions such as diabetes mellitus, heart disease, hypertension, asthma, tuberculosis, CVA, anemia, hemophilia, arthritis, cancer, and any other condition the client can list. Assess the family’s general physical health, general emotional health, and family situation.
ACTIVITIES OF DAILY LIVING (ADL)
Assess if the client is independent, dependent, or requires assistance with ADLs for each area. If assistance or assistive devices (walkers, w/c (wheel chair), plate guard, etc.) are required, describe and when/how they are used for increased dependence. Evaluate the following areas:
Mobility: Is the client mobile by ambulation, w/c, in bed, and during transferring.
Dressing/Undressing: Can the client dress for the day, for the night, and what is the usual clothing that he/she wears.
Sleep: What are the usual hours of sleep? Are naps usually taken and what sleeping aids are used?
Hygiene: Does the client prefer a shower, bed bath, or tub bath and is there a preference for a.m. or p.m. Do they use powders, ointments, or lotions? Assess the ability to perform oral care, peri care, shampoo, and styling of hair.
Recreation: Describe the type of work, educational level, leisure activities, fatigue/endurance levels of the client.
Diet and Elimination: Assess the client’s appetite (in percentage), eating ability or difficulties, usual diet, likes/dislikes and fluid intake/day. Also evaluate the client’s usual elimination pattern, recent elimination changes, aids used for elimination and last BM.
Miscellaneous: Are restraints required? Does the client use a prosthetic device, assistive equipment, etc?
ASSESSMENT
A notation must be made in every space. The * areas denote that these areas must have descriptive notations made. All other areas may have a (-) or a N/A noted if this abnormality was not found. If an abnormality is noted, check the condition and describe on the lines of explanation.
INTEGUMENTARY
Skin: *Assess for overall color, localized color, pigmentation, *temperature, eruptions, pruritis, ecchymosis, dryness, diaphoresis,
rashes, lesions, infection, wounds, moles/scars, ulcerations, lacerations, avulsion, pressure areas, ulcerations and *turgor.
Hair: Dry brittle, *distribution.
Nails: Brittle/soft or abnormal nails, *nailbed color.
Misc.: Heat/cold intolerance.
HEAD
Trauma, lumps, alopecia, cephalgia
Eyes: Near sighted/far sighted, corrected with glasses/contacts, glaucoma, cataracts, blurring of vision, burning, itching, photo
phobia, pain, edema, excessive tearing, and diplopia.
Ears: Hearing loss, vertigo, tinnitus, pain, ear infections, drainage, hearing aids
Nose: Discharge, colds, sinusitis, epistaxis, obstruction, trauma, breathing problems, deviated septum, rhinitis, smelling ability
diminished.
Mouth/Pharynx: Loss of teeth, dental caries, toothaches, mucous membrane abnormalities – should be moist and intact, tongue
deviations, halitosis, voice changes, dysphagia, hoarseness, oral lesions, dentures/bridges, and loss of taste.
NECK
Limited movement, pain, stiffness, thyroid problems or goiter.
RESPIRATORY
*Respiratory rate, *depth, chest movement non symmetrical, use of ancillary muscles, dyspnea, SOB, nasal flaring, pain, orthopnea, cough-productive? If so, then sputum color, amount and frequency; hemoptysis, abnormal breathing pattern, cyanosis/pallor, and stridor. *Auscultation: rales, rhonchi, wheezes, or pleural friction rub.
CARDIOVASCULAR
Pulses – Look at *rate, *rhythm, and *quality of pulse: carotid, *radial, *apical, femoral, popliteal, post tibial, and *dorsalis pedis.
Assess for chest pain, palpitations, arrhythmia, capillary refill, cyanosis/rubor/pallor, varicosities, *skin temperature, claudication, phlebitis, *peripheral edema, and Homan’s sign.
B/P: Should check at least 2-4 of these B/P, based on other S&S and medical/nursing diagnosis:
*R: lying _____ sitting _____ standing
*L: lying _____ sitting _____ standing
GASTROINTESTINAL
Diet – dysphagia, n/v, heartburn, flatulence, pain, jaundice, mass, distention, ascites, hemorrhoids, rectal bleeding, recent weight loss/gain, *bowel sounds – hypo/hyperactive – noted in all 4 quadrants, *character of stool, and evaluate any change in bowel patterns, *when was last stool?
URINARY
Frequency, polyuria, oliguria, nocturia, dysuria, dribbling, pyuria, retention, infections, perineal rash, urgency, and *character of urine.
REPRODUCTIVE
Perineal lesions, discharge, contraceptive practices, STDs.
Male: Prostatic problems, loss of sexual function.
Female: *Gravida (pregnancies), *para (births), irregular bleeding, dysmenorrheal, dysparenuria, *last normal menarche or date of menopause, *last Pap test, loss of sexual function.
MUSCULOSKELETAL
Pain in joints or muscles, deformities, gait, weakness, limited ROM, contractures, paralysis, activity intolerance, and *posture.
NEUROLOGIC
Cephalagia, seizures, dizziness, fainting, tremors, paresthesia/paralysis, ataxia, pupils (size and *PERLA), *hand grasps (strength and equality), *level of consciousness (1-5 stages), oriented x 3 (*person/place/time), recent/remote memory loss, neuralgia, any posturing (abnormal extension/flexion).
PSYCHOLOGICAL
Anxious, angry, fearful, uncooperative, irritable, dependent, demanding, any affect problem (flat, depression, mania), abnormal behaviors, delusions or hallucinations.
*DIAGNOSTIC TESTS
Test Norm values Interpretation and Implementations
List all the lab work on the chart – if it is within normal range, you may just write WNL (within normal limits). However, if it is not WNL, please write in the client’s values, the normal values, and your interpretations of what this result is indicative of. Also write in how this will alter the nursing plan of care/your nursing interventions.
*PHARMACOLOGY
Meds Dose Route Times Classification
List all the medications that the client is taking; OTC, and all prescribed meds. Also write information regarding the client’s IV therapy.
*TEACHING OPPORTUNITIES
Make note of all the teaching that you will do for the client. This includes formal prescribed teaching as well as opportunity/bedside teaching. List when, how, what, and why you will teach.
Name: Date:
NURSING ASSESSMENT
Client initials: Room: Doctor:
Primary Dx:
Secondary Dx:
Ethnic Identity: Marital status: Age:
Religion: Language: Gender:
Admission Date: Special Needs? Allergies:
Current medications:
Routine
PRN
IV
Chief complaints:
History of present illness:
Vital Signs T P R B/P
1.
2.
Orders:
Activity level:
Diet:
Therapies:
Special Nursing Procedures:
HISTORY
Past history:
Psychosocial history:
Family history:
Heredity conditions/general physical health/general emotional health/family situation
ACTIVITIES OF DAILY LIVING
I = independent A = assistance required D = dependent
Mobility
Ambulatory w/c bed transfer gait
Notes:
Dressing/Undressing
Dressing for day dressing for bed usual dressing
Sleep
Usual hours of sleep naps sleeping aides
Hygiene
Shower bed bath bathtub a.m. p.m. powders/ointment/lotions preferred
Oral care peri care shampoo styling
Recreation/Activity
Type of work education level leisure activities Fatigue/endurance
Diet/Elimination
Appetite eating ability usual diet likes/dislikes
Fluid intake/day elimination pattern aids used for elimination
Elimination changed recently? Explain yes: *last BM
Misc: restraints prosthetic device call light available assistive equipment
PHYSICAL ASSESSMENT
Integumentary
*Color – overall localized hair skin temp
*nails and nail beds diaphoresis heat/cold intolerance *turgor
Other Explain:
Head
Trauma masses alopecia cephalalgia other
Eyes
*Vision corrected? Glaucoma cataracts pain edema tearing
Other
Ears
Hearing loss aids vertigo tinnitus pain ear infections
Drainage other
Nose
Discharge/drainage obstruction smelling ability diminished other
Mouth/Pharynx
*Teeth dentures/bridges dysphagia *mucous membranes hoarseness
Voice changes loss of taste other
Neck
*Movement pain thyroid problems other
Explain:
Respiratory
*Respiratory rate *depth *symmetry use of ancillary muscles dyspnea
SOB nasal flaring stridor orthopnea cough sputum
Abnormal breathing pattern cyanosis/pallor hemoptysis pain other
*Auscultation: rales rhonchi wheezes friction rub other
Explain:
Cardiovascular
Pulses (rate, rhythm, quality): carotid *apical *radial femoral popliteal
Post tibial *dorsalis pedis chest pain palpitations arrhythmia *capillary refill
*color/cyanosis/rubor/pallor varicosities Homan’s sign *skin temperature
Claudication phlebitis peripheral edema other
B/P *R: lying sitting standing
*L: lying sitting standing
Explain:
Urinary
Frequency polyuria oliguria nocturia dysuria dribbling pyuria
Retention infections perineal rash urgency other
*character of urine Explain:
Reproductive
Perineal lesions discharge contraceptive practices STDs other
Male: Prostatic problems
Female: *gravida *para irregular bleeding dysmenorrhea dyspareunia
Last normal menarche date of menopause last *Pap
Explain:
Musculoskeletal
Pain in joints pain in muscles redness deformities gait problems
Weakness limited ROM contractures paralysis activity intolerance
*Posture other Explain:
Neurologic
*Level of consciousness tactile sensing cephalalgia convulsions dizziness
Fainting tremors paresthesia/paralysis ataxia aphasia *pupils
*hand grasps *alert *oriented to person/place/time recent/remote memory loss
Neuralgia posturing other Explain:
Psychological
Self esteem alteration ______anxious ______angry ______fearful ______uncooperative ______
irritable ______dependent ______demanding ______affect problem ______
delusions ______hallucinations ______other ______
Describe behaviors:
*DIAGNOSTIC TESTS
Test Norm values Interpretation
CBC:
WBC
H & H
Platelets
UA
Blood Glucose or Accu-Check
C & S
Chemistry:
Electrolytes
BUN & Creatinine
ABG’s
X-Ray
Other
TEACHING OPPORTUNITIES
Instructions & Nursing Assessment
Reviewed: 10/05, 9/06, 2/07, 3/07, 9/07, 4/08, 10/08