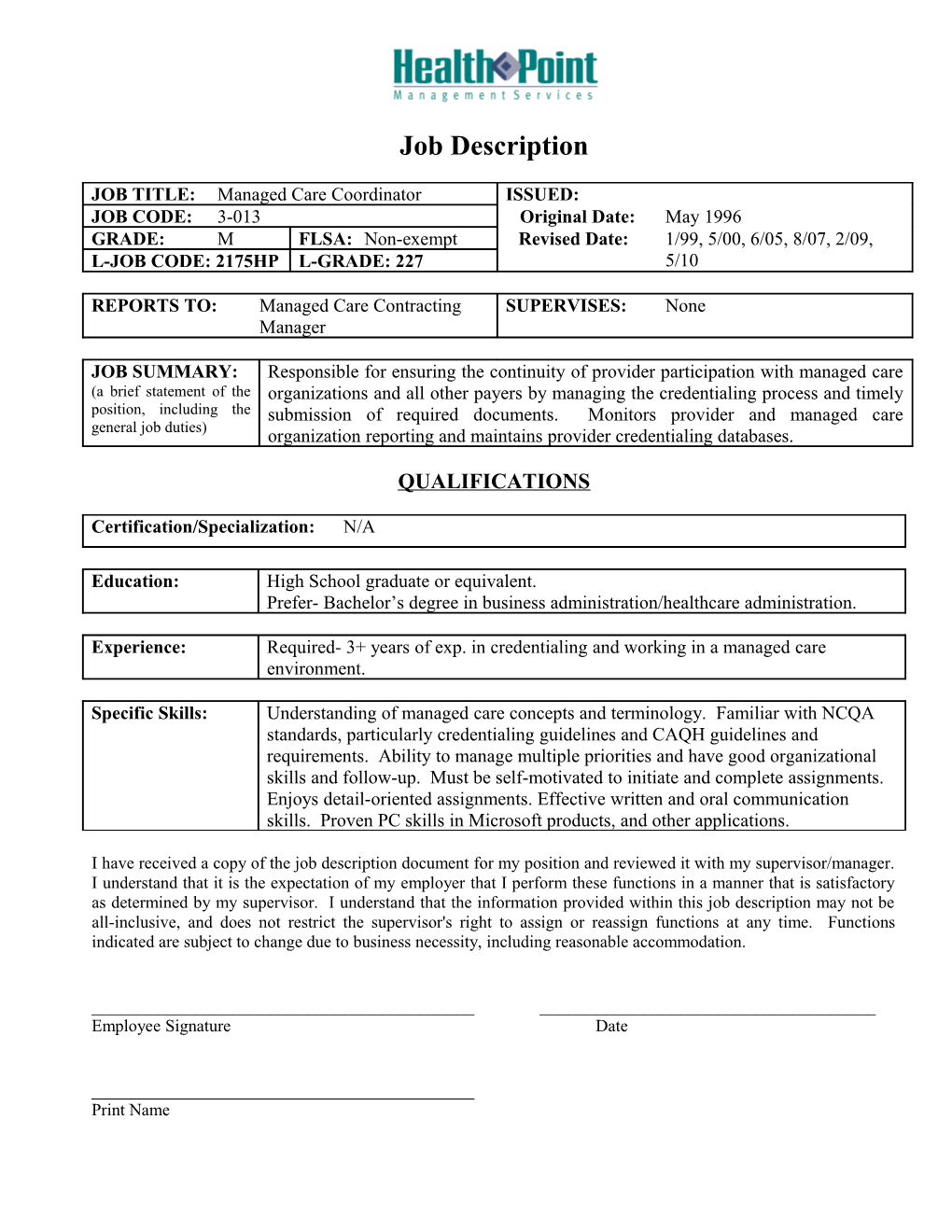
Job Description
JOB TITLE:Managed Care Coordinator / ISSUED:JOB CODE:3-013 / Original Date:May 1996
GRADE:M / FLSA:Non-exempt / Revised Date:1/99, 5/00, 6/05, 8/07, 2/09, 5/10
L-JOB CODE: 2175HP / L-GRADE: 227
REPORTS TO: Managed Care Contracting Manager / SUPERVISES:None
JOB SUMMARY:
(a brief statement of the position, including the general job duties) / Responsible for ensuring the continuity of provider participation with managed care organizations and all other payers by managing the credentialing process and timely submission of required documents. Monitors provider and managed care organization reporting and maintains provider credentialing databases.
QUALIFICATIONS
Certification/Specialization:N/AEducation: / High School graduate or equivalent.
Prefer- Bachelor’s degree in business administration/healthcare administration.
Experience: / Required- 3+ years of exp. in credentialing and working in a managed care environment.
Specific Skills: / Understanding of managed care concepts and terminology. Familiar with NCQA standards, particularly credentialing guidelines and CAQH guidelines and requirements. Ability to manage multiple priorities and have good organizational skills and follow-up. Must be self-motivated to initiate and complete assignments. Enjoys detail-oriented assignments. Effective written and oral communication skills. Proven PC skills in Microsoft products, and other applications.
I have received a copy of the job description document for my position and reviewed it with my supervisor/manager. I understand that it is the expectation of my employer that I perform these functions in a manner that is satisfactory as determined by my supervisor. I understand that the information provided within this job description may not be all-inclusive, and does not restrict the supervisor's right to assign or reassign functions at any time. Functions indicated are subject to change due to business necessity, including reasonable accommodation.
______
Employee SignatureDate
______
Print Name
Managed Care Coordinator
PERFORMANCE INDICATORS
I.ESSENTIAL FUNCTIONS
A.Quality Philosophy and Process
1.Demonstrates dignity, respect, excellence, trust and responsibility in all actions.
2.Speaks positively about the organization and its team members and services.
3.Understands and participates in quality and process improvement activities.
- Customer Service Expectations
1.Attempts to exceed customer expectations by complying with published HealthPoint Service Expectations.
2.Acknowledges customers promptly and courteously, creating a welcoming environment.
3.Demonstrates proper written, telephone and electronic communication courtesy and etiquette (i.e., promptly returns voicemails and emails).
4.Uses time productively, coordinating with others, to achieve common goals and objectives.
- Takes responsibility to promote team work and professionalism; completes own work efficiently and accurately and then assists co-workers with theirs.
- Takes pride in working for HealthPoint; promotes a positive image of HealthPoint through words and actions.
C.Team Member Responsibility
- Consistently demonstrates a full understanding of our Mission and Values.
- Promotes a safe and secure environment; engages in proper safety and infection control practices.
- Recognizes and adheres to the Corporate Responsibility (“Doing the Right Thing”) and HIPAA Guidelines, including confidentiality.
- Complies with organizational and department policies and procedures including attendance, behavior, dress code, productivity and required meetings.
- Completes all required training including maintaining competencies.
- Welcomes new employees and helps orient them to practice/dept.; encourages questions and new ideas.
II.JOB SPECIFIC FUNCTIONS
- Provider Credentialing Applications.
- Maintains physician credentialing files.
- Verifies provider information for Delegated Credentialing - request all primary source verification (i.e. NPDB, education, training, hospital privileges, etc.) and verify licensure, Board Certification etc.
- Reviews credentialing file for accuracy and completion and submits to Managed Care Contracting Manager and Medical Director for review in preparation for Credentialing Committee meeting.
- Coordinate and review site visits for each site annually.
- Prepares meeting minutes for Credentialing Committee meeting
- Submits notice to providers of Delegated Credentialing Approval
- Submits notice to plans of providers approved, terminated or modified under Delegated Credentialing.
- Coordinates scheduling of and assists plan representatives during credentialing audits.
- Submits completed credentialing and re-credentialing applications to non-delegated ManagedCare Organizations (MCO) and other non- delegated payers.
- Completes Medicaid/Medi-Pass and Medicare credentialing and re-credentialing applications.
- Follows-up with provider relations representative of insurance plans to facilitate prompt completion of credentialing.
- Tracks credentialing status and meets with Managed Care Contracting Manager regularly to report issues.
- Responds to general inquires from insurance plans, hospitals and sites
- Facilitates/processes physician hospital privileges applications for new providers.
- Processes hospital re-credentialing applications for providers.
JOB SPECIFIC FUNCTIONS continued
- Performs assigned tasks related to new providers transitioning into the Group and providers leaving the Group.
- Renews Providers licenses and DEA’s.
- Creates, updates and maintains NPI registration for Groups and providers in NPPES database.
- Databases and Reports.
- Updates and maintains credentialing database.
- Maintains Credentialing Policies and Procedures; proposes changes and updates file with approved changes.
- Updates, maintains and distributes Managed Care Matrices.
- Updates insurance plan mailing list.
- Develops and distributes approval notifications promptly.
- Facilitates development of provider reporting.
- Establishes and maintains other databases to support the Managed Care Department.
- Maintains NPPES, CAQH, Medicare PECOS, and Florida License databases.
- Professional Relations.
- Participates in professional development activities and maintains professional affiliations.
- Communicates effectively with physicians, office and administration personnel in order to share information and problem solve in an effective manner.
- Uses time productively coordinating with co-workers to achieve common goals and objectives.
- Maintains open communication with Manager of Managed Care Contracting, status of assigned projects.
- Liaison between the practice sites to the health plans regarding problems/issues.
- Notifies health plans of Practice changes (i.e. panels).
- Completes Provider Information Forms for distribution.
- Assists Managed Care Contracting Manager as needed.